Introduction
Asthma is a lung disease. Asthma causes the breathing tubes in the lungs to temporarily narrow. People with asthma have difficulty breathing air in and out of their lungs. An allergen or irritant in the environment usually triggers an asthma flare-up.
There is no cure for asthma. Some asthma flare-ups can be prevented. Asthma can be treated with lifestyle changes and medication. Untreated asthma can become severe and life-threatening. People can control their asthma with self-management and medical treatment.
Most people with asthma can lead normal lives.
Anatomy
Your lungs are located inside of the ribcage in your chest. Your diaphragm is beneath your lungs. The diaphragm is a dome-shaped muscle that works with your lungs when you breathe.
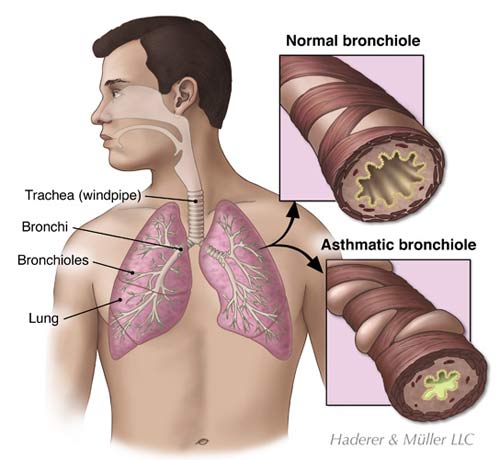
From your nose and mouth, air travels towards your lungs through a series of tubes. The trachea or windpipe is located in your throat. The bottom of the trachea separates into two large tubes called the main stem bronchi. The left main stem bronchus goes into the left lung, and the right main stem bronchus goes into the right lung.
Once in the lung, the bronchi branch off throughout the lung and become smaller. These smaller air tubes are called bronchioles. There are approximately 30,000 bronchioles in each lung. The end of each bronchiole has tiny air sacs called alveoli. There are about 600 million alveoli in your lungs. Each alveolus is covered in small blood vessels called capillaries. The capillaries move oxygen and carbon dioxide in and out of your blood.
When you breathe air in or inhale, your diaphragm flattens and your ribs move outward to allow your lungs to expand. The air that you inhale through your nose or mouth travels down the trachea. Tiny hair-like structures in the trachea, called cilia, filter the air to help keep mucus and dirt out of your lungs. The air travels through the bronchi and the bronchioles and into the alveoli. Oxygen in the air passes through the alveoli into the capillaries. The oxygen attaches to red blood cells and travels to the heart. The heart sends the oxygenated blood to the cells in your body.
When you breathe air out or exhale, the process is the opposite of when you inhale. Once your body has used the oxygen in the blood, the deoxygenated blood returns to the capillaries. The blood now contains carbon dioxide and waste products that must be removed from your body. The capillaries transfer the carbon dioxide and wastes from the blood and into the alveoli. The air travels through the bronchioles, the bronchi, and the trachea. As you exhale, your diaphragm rises and your ribs move inward. As your lungs compress, the air is released out of your mouth or nose.
Causes
Asthma causes the bronchial tubes in the lungs to swell and become narrower. The muscles in the airways contract causing even further narrowing. The bronchioles may also produce extra sticky secretions or mucus. Asthma makes it harder for a person to inhale or exhale.
Doctors do not know exactly what causes asthma. They do know that the airways in some people are sensitive to triggers that cause an asthma flare-up or “asthma attack.” Allergens are a type of trigger that causes allergic reactions in the airways. Common allergens include pollen, pet dander, dust mites, mold, cigarette smoke, polluted air, perfume, and cleaning products. Triggers may also include cold dry air, physical exercise, stress, nonsteroidal anti-inflammatory drugs, and sulfites, a type of additive found in food or wine. Some people experience asthma when they have a cold, the flu, or bronchitis. Laughing or crying can even trigger asthma.
There are different types of asthma. Adult-onset asthma begins after the age of 20. Exercise-induced asthma occurs during exercise that requires breathing through the mouth, continuous activity, or cold weather. Occupational asthma involves exposure to irritants at the workplace. Such irritants may include chemicals, plastics, rubber, paint, and metal products. Nocturnal asthma occurs between midnight and 8 AM. It is triggered by allergens in the home or sinus conditions.
Symptoms
Most people with asthma have periodic flare-ups and symptom-free periods. Some people have difficulty breathing all of the time and periods of very difficult breathing. Asthma flare-ups can last from minutes to days. They can be very dangerous if the airway is severely restricted.
Asthma makes it difficult to breathe. You may have to work extra hard to breathe under normal conditions. You may experience shortness of breath that is made worse by exercise.
You may hear a wheezing sound when you breathe. Wheezing sounds like a whistle or high-pitched musical noise. It is caused by air being forced through the narrow airways. Wheezing usually begins suddenly. It may come and go. It may occur more often in the night or early morning hours. Cold air or exercise may cause wheezing to increase. Wheezing may be accompanied by a cough. It is important to note that not all people with asthma wheeze, and not all people who wheeze have asthma.
You may also experience nasal flaring, chest pain, or chest tightness. It may take you longer to breathe out than it does to breathe in. You may have an uneven breathing pattern with temporary stops. It may be difficult for you to speak.
Symptoms of severe asthma are signs of a medical emergency and may lead to death without treatment. You should call emergency medical services, or have someone drive you to a hospital emergency room if you experience an extreme difficulty with breathing. Other emergency symptoms include sweating, a rapid pulse, and anxiety associated with shortness of breath. Additionally, your lips and face may appear blue.
Diagnosis
Your doctor can diagnose asthma by reviewing your medical history and conducting a physical examination and tests. You should tell your doctor about your symptoms, risk factors, and what appears to trigger your asthma flare-ups. Your doctor will listen to your chest while you breathe. If you are experiencing an asthma episode, your doctor may hear wheezing. However, wheezing is not present between asthma flare-ups. There are several tests that your doctor may conduct to find out the cause of your symptoms and the degree of your airway obstruction. Your doctor may also order a chest X-ray to rule out other conditions that have similar symptoms.
Your doctor will have you breathe into a hand-held device called a spirometer. A spirometer measures how much air you breathe out and how forcefully you breathe the air out. Your doctor will also have you breathe into a peak flow meter. A peak flow meter is a hand-held device used to manage asthma by monitoring the airflow through your bronchi. The peak flow meter measures your ability to expel air from your lungs under the best or peak conditions. Your rates will be higher when you are feeling well and lower when you have an asthma flare-up. By monitoring the changes in your breathing patterns your doctor can identify how well your lungs are functioning, the severity of your symptoms, and appropriate treatment.
Your doctor may use a pulse oximeter to determine the amount of oxygen in your blood. For this test, a probe will simply be placed on your fingertip. A medical device attached to the probe displays the percentage of oxygen in your blood.
Your doctor may take a sample of your blood to determine the amount of carbon dioxide and oxygen in your blood. A blood test may also be used to identify infections or other causes of your symptoms. Additionally, a blood test or skin test may be used to determine the type of allergies that you may have.
Asthma is classified as Mild, Moderate, or Severe according to its severity. People with Mild Asthma have symptoms that occur twice per week or less. The symptoms are quickly relieved with medication and there are no symptoms in between episodes. People with Moderate Asthma experience symptoms every day. They require inhaler medication almost every time for symptom relief. Severe Asthma causes symptoms for the majority of every day. People with Severe Asthma may need to restrict their activities. They may need a hospital stay for treatment.
Treatment
The goals of asthma treatment are to establish normal lung function, relieve symptoms, and prevent asthma flare-ups. There is no cure for asthma, although symptoms may decrease over time. It is important to identify and avoid the allergens that trigger your asthma. Your doctor may prescribe medications based on your condition.
The type of medication that you receive depends on the severity of your asthma, the cause of your symptoms, and your lung functioning. You may receive long-term medications or quick relief “rescue” medications. Long-term medications are used on a regular basis to prevent asthma. People with persistent asthma flare-ups use long-term medications to prevent symptoms. Quick-relief medications are used during an asthma flare-up to relieve symptoms. People with Mild Asthma or infrequent flare-ups may use quick relief medications as needed.
Your doctor will instruct you on how to use a peak flow meter at home. By measuring your lung volume, you may be able to detect an upcoming asthma flare-up and take action according to your doctor’s instructions. Using a peak flow monitor can prevent an asthma flare-up from taking you by surprise.
Prevention
You should wear a MedicAlert bracelet and carry a MedicAlert card in your wallet. In the case of an emergency, the MedicAlert information will be helpful to the healthcare professionals treating you. Because the medical complications associated with asthma can be very serious, people with asthma need to diligently manage their condition to remain healthy.
You should formulate a plan with your doctor as to what you should do in the case of an emergency or serious situation. You should know how to use your medication properly and when to use it. You should also know what to do if your medication does not work right away and when to go to the emergency room near me.
You may be able to prevent or reduce your asthma flare-ups by avoiding the triggers that cause it. Talk to your doctor to find out if allergy treatments are an option for you. You may also make lifestyle changes to protect yourself from allergens. This may include staying indoors when pollen levels are high or removing carpets from your home. Ask your doctor for recommendations that are appropriate for you.
Learn how to use a peak flow meter at home. Check your peak flow regularly. Keep a record of your results and bring them to your doctor’s appointments. The record will help your doctor to monitor your medications. Additionally, make sure that you attend all of your doctor appointments.
Am I at Risk
About half of all asthma cases occur in children under the age of ten. Boys are more likely than girls to develop asthma. Conversely, women are more likely than men to develop adult-onset asthma. Asthma affects people of all races. It is more common in people who are Afro-American or Hispanic.
Risk factors for asthma:
_____ Smoking or living with a smoker can increase your risk because smoke is unhealthy for the lungs and can be an asthma trigger.
_____ A family history of asthma. If your parents, brothers, or sisters had asthma, you have an increased risk of developing it as well.
_____ If you have allergies or eczema, or a skin condition, you have an increased risk of developing asthma.
_____ If you had allergies or a severe viral infection before you were three years old, you are at risk for developing asthma.
_____ Living in the inner city or being exposed to mice and cockroach waste products increases your chance of developing asthma.
_____ If you are frequently exposed to triggers, you are at risk for asthma.
Complications
Complications from asthma can lead to hospitalization and even death. You may be hospitalized if your asthma is very severe or does not respond to treatment. You may be hospitalized if you develop a serious lung illness or a pneumothorax, a collapsed lung. Other conditions that warrant hospitalization include poor lung function and elevated carbon dioxide or low oxygen levels in the blood. The hospital staff will monitor and treat your condition. Some people may have to be placed on a ventilator, which is a machine that can breathe for them.
